Updated October 10: Added transcript of the video, at bottom.
On Tuesday morning, my Dutch colleague Lucien Engelen (Twitter @LucienEngelen) took me to the production studio in the attic of his little office and we shot this interview. I had no idea what questions he’d ask, and this was my day for jetlag confusion after a Saturday night redeye from the US. He edited it down, and boom, instant TV show! I’ll explain the context in a moment, but first, the interview (13:37):
Here’s a companion article (in Dutch) in Thursday’s “Skipr” (Dutch health newspaper) about REshape, including this video and an audio interview (also in Dutch) with Lucien.
The setting: Radboud REshape Center
I’m in the Netherlands this week, for a series of events at “UMCN” – University Medical Center at Nijmegen. It’s the oldest city in the nation, an hour southeast of Amsterdam. (Here’s the Wikipedia article in Nijmegen, including this “Listen” link for pronunciation.)
In the Netherlands UMC is analogous to the American AMC / academic medical center; this one is at Radboud University Nijmegen, named for St. Radboud. As the REshape site describes, one of their projects is “REshape Academy,” founded and funded by the hospital’s board. (Get this: these visionary board members are not only successful business people, they’re tweeps, including new CEO @MelvinSamsom and @C@CCVanBeek!)
REshape is action oriented.
The e-Patient Boot Camp
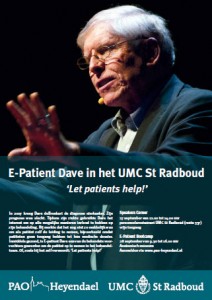
When I announced my plans for 2011, a key objective was to launch a seminar product. This Wednesday we did the first one – “e-Patient Boot Camp EU.” It’s an intensive six hour day that combines many of the topics I’ve spoken about in the past two years, with group discussions to develop specific next actions. At right is the poster they created for the event.
The Boot Camp, two departmental consultations, and the interview below were all organized by a project attached to the UMC, the Radboud REshape Center: (Emphasis added)
REshape is a program set up by the Radboud University Medical Centre in Nijmegen. Our aim is to fire up and grow a movement of people who believe the next decennium should be the era of the rising of self-empowered patients, in which we will embrace the patient, their family and informal care into the healthcare team.
We nurture the movement by setting up conferences to exchange thoughts, visions and listening to each other. But also by doing research on the different aspects of participatory healthcare which helps to move forward. As a vehicle for the (needed) changes, we are scouting, inventing and sharing innovations (inter)nationally to improve healthcare.
Lucien Engelen is an energetic entrepreneurial visionary if I ever saw one. He’s constantly full of ideas, usually laughing and excited, and boy does he know how to make things happen. Like some other great healthcare innovators I’ve seen, he was successful in other fields before setting his sights on medicine.
I hope to post more on the week’s four other events.
(If you want to sponsor an e-Patient Boot Camp for your community, or for sale to the public, reach me at the Contact page here.)
___
Transcript of the video
Edited a bit for clarity
We are at a magnificent point – I say a turning point – in the history of this movement. There have been people for more than 10 years who been actively involved in taking some early principles – like when Dr. Spock in the 1940’s, in his baby book, told parents, “Trust yourself. You know more than you think you do” – and other people have moved this forward over the decades.
We are now at a point where we are starting to formalize what we mean by patient empowerment and patient engagement. What’s possible in that area is radically altered by the introduction of the internet, particularly the web in 1994, and now by health IT moving forward, which makes it infinitely more possible, more feasible than before, for patients to look at their medical records, their families’ medical records, to be actively involved.
So now, as I’ve been speaking for the last couple of years at all sorts of different conferences, we’ve gotten to the point where people are saying, “Okay I get it – I see this is possible.” And as our costs keep rising and the patient load keeps rising as the baby boomers age, now the question is, what do we do about [patient engagement]? How do we get to work? How do we make this reality? How do we take what’s possible and turn it into the new reality? And that’s what the boot camp is about.
Boot camps are about basic training – getting yourself up to speed and getting started.
Second clip:
It is an extraordinary evolutionary turning point, again, to use that term.
I am alive because of phenomenal technical achievements in medicine. When I discovered in 2007 I was almost dead with kidney cancer, my median survival at the time was 24 weeks. And that really focuses the mind and makes one appreciate the skill of brilliant people who know how to stop that process in the body.
The high dosage interleukin-2 treatment that I got was developed as part of the phenomenal explosion of new technologies during my lifetime. I was born in 1950; the polio vaccine was just barely coming on the scene – nobody could imagine something like cat scans, which are now routine, not to mention on top of that all the biological innovations, as we’ve come to understand DNA and cellular processes and all that.
So for a while there was incredible value being generated in the biological or technical aspects of health care. [But] the seesaw just tipped, and to some extent, the human aspect, the human touch, the ability of somebody to sit down and look you in the eye and say “How are you doing?” You know, “How’s it going?” has been deprioritized. And I don’t know if it’s that we reach the sort of saturation point of how much more value there is in more technology, or if it’s just that we’ve started to feel more and more the hunger for the touch, the human physical or social touch aspects.
I know when I was in the middle of my treatment and the odds were that it was not going to work, and I was on my way out, that’s an extraordinary place to be. It’s like hanging half off the edge of a cliff. And there are people who come – the nurses – nurse practitioners and occasionally doctors who would come stand at the foot of my bed, I don’t know how they did it given that they have [other patients too] … they just went from patient to patient to patient, [but] when they stood there– it was like there was nobody else in the world in their attention. They were just with me, listening to me. And I felt cared for.
Now, it’s funny … I mean, I’m a technologist – I’m all for IT and what new gadgets can do – but I haven’t seen a care gadget yet – something that gives me the sense that I’m connected to a caring person. So I’m looking forward to [pause]… maybe it’s a maturing process, where we learn to take this new stuff – like, “OK, we got that down – we’re good at that, we can do things that were simply not possible 50 years ago,” and now weave that into the fabric of a caring relationship.
Third clip:
When I was facing death and [pause] … as rational and technologically minded as I am, the right brain part of me was sort of afloat, you know? adrift in space. And I read things, and I remembered things I’d read, about death – what that transition would be like. And I also recalled times in my life when I just felt a deep silent connection with somebody. I don’t know what that is and if we’ll ever completely be able to measure it, but I am confident that it’s there and it’s real.
And we also know now there’s some evidence that patients who have a good level of social connectedness do better in recovering from illness. I’m starting to think about it in terms of a broader context of well-being – and I don’t mean well being in the usual sense of fitness and so on, but being well. And I’m pretty sure that there’s a strong component of that that has to do with connectedness. So for somebody to offer me any kind of support, technological or otherwise, while being connected in a nurturing way somebody wanting me to be well, makes a big difference.
I think there’s a business aspect to that also because I’m fund of saying that health care is the only industries I ever seen where the definition of quality doesn’t start by considering, “What does the customer want?” Now we can think about that in terms of lab results, or “I want a wheelchair readily available when I step in the door of the hospital.” But we can also think about it in terms of – if we define value in healthcare as moving from wherever a person is now, with a problem, to a state of being well, then that’s very different things that … you know, treatment, surgery, whatever, that alter our tissue are one thing; but there’s a whole spectrum of things that are in addition to that. And as I say I’m very happy that the ability to alter our tissue is very well developed because without that I wouldn’t be alive to today.
Q: Looking to the things that you’ve done up until now and your plan for the next 2 years, what will change?
A: Well, that’s funny – it’s hard to ask a 20 year old what they plan to do for the next 20 years, because the 20 years that they’ve just been through bears no resemblance to the 20 they’re entering. And I’ve been involved in health care – observing care, trying to figure out what could I say that would be useful, what could anyone do that would be useful – for 2 years. So over the next 2 years I really don’t know what life’s going to look like.
And having said that, based on the feedback that I get from the people that I’ve met, it is time to build out the practices and principles. It’s time to hypothesize about what might work. Start trying some things.
I very, very much want to connect with as many other engaged patients, e-patients as I can, from around the world. Some people think I invented this field. That’s ridiculous – I got interested in it, and I speak about it, but I got interested in it by reading the e-patient white paper, about what people had been doing for 10 or 20 years. And now I’m just finding more and more and more people who’ve been doing it. What’s their experience? What can we do to harvest all of that knowledge and have them start trying things in their world and connecting – sharing experiences to see what works.
There’s a major economic driver here. In the US costs are spiraling up (my impression is that in other countries they are becoming greater too), cost per individual. And that’s compounded by the [number of] boomers who are entering the high consumption phase. So two things will be happening, [and] there’s going to be much higher cost net – the total cost of treatment being done.
And we’re going to have more and more cases where people simply can’t afford to have the utmost done for them, so they’ll be facing a question of, okay, in the same way that I don’t live in a penthouse suite in the Alps, or something like that… [people will have to ask themselves] “what can I do that will suit my needs and be fulfilling?” There will be people facing care choices …
Some people would say – economists might say – that this is a good thing, because you have goal congruency, where the person consuming the services has a stake that is aligned with the society’s. But I assert that you can’t do that effectively or ethically unless the people who are newly making these decisions are sufficiently informed and have sufficiently developed skills, so that they do it well. Because otherwise you’ll just have people falling off the bicycle and nothing will improve.
But that’s it! So let’s get to work.
Interviewer: Thank you. Thank you. [Laughs] That’s one. So this is a cut. [Laughs]
Q: My perspective on reshaping healthcare is different from anything I’ve heard from all of the people who are saying good things about patient centered care.
Very often those arguments for change are about thinking more about what people want, which is a good thing. But I think at a deeper level there’s an issue of, “How can it be that so many smart, hardworking, motivated, sincere, high integrity people have worked so hard for decades and we haven’t manage to substantially improve the value proposition?” You know? The value that patients get out of healthcare has not improved anywhere near proportional to the costs.
[So] to me, it seems like that’s because we’ve been changing the wrong tire on the car over and over again. We’ve been working on better, more efficient means of delivering services but that’s not where the problem is. To me the problem is that we just haven’t been thinking enough from the perspective of the humble supplicant saying, “Please help me.”
And that’s, to me, that’s what reshaping care is. It’s not taking all the machines and laboratories and turning them so that they’re pointed at the patient, it’s rethinking the whole thing from what will really make people’s lives better. Because that, then, will give us focus on how to prioritize the rest.
Question on the screen: What do you think of the process set up at RUNMC? [Radboud University Nijmegen’s Medical Center]
A: When I started out 2 years ago and really got focused a year and a half ago on making a new career in healthcare because I’d just found this calling, I knew I was completely ignorant, innocent you know, in my first 6 months or so I had to start every talk by saying “I’m completely humble to be here, I’ve no idea what I’m talking about, about healthcare at large, I just know my own experience.”
Well, since then through whatever mysteries of the universe, I’m spoken at over 150 events – I just counted it up recently – and I’ve seen a lot of different perspectives on what’s the nature of the problems and what should we do about them. I haven’t seen anything, anywhere that as cleanly identifies that the task is to truly reshape healthcare like remolding a piece of clay in a way that’s entirely focused on what patients need.


Terrific interview, Dave. Nothing like jetlag-confusion – rather, beautiful articulated what many of us are working towards for decades. It is amazing how many initiatives are emerging in different parts of the world. We sometimes come from different background and perspectives – as you know, my personal angle is one of an evidence-based approach and collecting data on what works and what doesn’t, by creating the JMIR journal (http://www.jmir.org) and the Medicine 2.0 Conference Series and Network (http://medicine20.net) – but in the end we are all pulling on the same string and I agree that vast progress has been made in the past 5-10 years with this kind of thinking almost becoming mainstream. Perhaps it is time for a network of networks. Good luck with your next 150 speaking engagements :-)
It is always exciting to hear from the movers and shakers in healthcare.. As Gunther pointed out many many people have been working on this for a couple of decades.. We already know what works actually though and you don’t need to try and create something new and it includes not only patients but providers and business models as well.
For me personally this started in the late 80’s when I left a job at microsoft to work in the AIDS community (everyone was dying) to implementing an EHR at group health (a co-op founded in the 1940’s with over 620,000 members now) that gave patients the ability to “WRITE” into their EHR before the doc’s could (they had view only access). One of their core values is to simply put the patient first and design out from there.
Thank you to both you and Gunther for doing the difficult work of speaking, traveling and hosting. I am just one of the many midwives out there committed to changing entire systems and hopefully helping to nurture the community.
Just as an aside I met Gunter at the recent Stanford #Med2.0 conference when I moved back from the front row to sit at his table without realizing who he was. His ability to embed patients and put them front and center in the event (as in prior ones) was a simple but very powerful example of how to change systems to allow the patients voice to be heard.