This is an exercise in “peer to peer health advice.” I’m asking for advice, from “the DOC” (diabetes online community) – more on that below.
Here’s a message I received from someone who’s really peeved about a technology for managing his Type 2 diabetes. Does your experience match his? Should his digital device match the results from finger sticks? If not, for heaven’s sake why?
I’ve completely lost confidence in the FreeStyle 14 day and Freestyle Libre readers and sensors I’ve purchased. The readings are all over the board. Most current examples:
- This morning, at 9:17 a.m., the reader alarm went off. I flashed the sensor which read 181. It made no sense why it was so high as I hadn’t even eaten. At 9:18 a.m. (two minutes later) I did a finger stick using the same reader and it read 119!
- Then, at 11:02 a.m., the sensor read 193. Two minutes later at 11:04 a.m., a finger stick showed 128.
I’ve also had the reverse happen, where the sensor showed me being low, while a finger stick showed I was in normal range. On several occasions, when I did not confirm with a finger stick, I’ve taken glucose tablets to correct the lows, likely inappropriately.
I have made medication changes based on these readings. My doctor has made medication changes based on the numbers generated by LibreView. I can’t tell you the number of times I’ve taken meds to normalize an offending number. Looking back, I have no idea if I was correcting an event that either didn’t need to be corrected or not correcting when I should have.
A LOT OF PEOPLE don’t take the time to verify the sensor’s #’s with a finger stick. Particularly in the middle of the night, and when the reader’s alarm doesn’t sound off.
____________
What do you think, people with diabetes? Have you seen experiences like this? Should the reader match finger sticks a few minutes later? (Again, I know nothing about blood sugar readings.) Is his experience to be expected? Is something wrong?
Peer to Peer Healthcare and the DOC
I’ve long said that diabetes has the archetypical e-patient community. By definition, successfully managing both Type 1 diabetes (where your pancreas can’t create your own insulin) and Type 2 diabetes (where you can’t consume the insulin your pancreas makes) requires being on top of things around the clock – specifically your blood sugar levels.
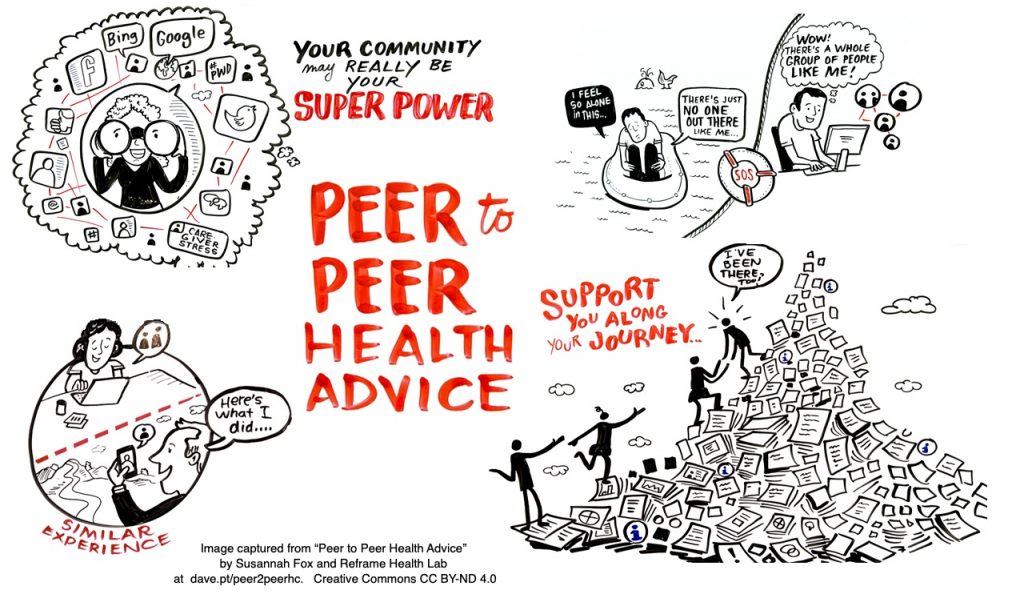
Not surprisingly, when social media came along, “the DOC” (diabetes online community) became a powerful source of what researcher Susannah Fox calls “peer-to-peer healthcare” [excellent 10 minute video], as people shared practical advice. At first “DOC” was a generic term, but now I discovered it’s become a slew of online communities and has even been the subject of several articles in scientific journals.
Then some people (not medical scientists, just people with diabetes and family & friends) created OpenAPS – their own software to digitally manage their insulin dosing, instead of doing finger sticks and tons of manual calculations and manual injections.
Who ever heard of patients inventing their own devices and software?? Well, that’s the concept I describe as Superpatients – patients who extend science, the book I’m trying to finish right now. To achieve that (which they have), they can’t be kidding themselves – they need to really be on top of things.
In any case, the DOC is a sharp bunch of people, so I’m asking their perspective on this fellow’s experience.


Discussion on Twitter (on day 1) has been tentatively helpful. I’ll paste in a few responses.
Friend David Harlow: “I am not an expert but CGM and fingersticks are measuring different things (interstitial fluid vs blood), and there’s a time lag in changes from one to the other.”
_________
@GingerViera:
“This has definitely been discussed in articles across the web, but it should be explained more clearly to patients the day they start using a CGM.”
“Doesn’t sound right. One is measuring glucose in interstitial fluid & the other in blood. Interstitial fluid is affected by food you just ate BEFORE your blood, so how close they are depends on when you last ate & how quickly your blood sugar is changing that moment. #mytwocents”
She added: “I hear ya!!! The technology is far from perfect, and diabetes education, too. Personally, this is a huge part of why I don’t wear a CGM — the inconsistencies create more anxiety and I take insulin when I don’t need, causing more fluctuations.”
@EusticeTheSheep posted a link to Diabetes UK’s page on CGM: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/testing/continuous-glucose-monitoring-cgm
@Shnoune posted several comments:
The numbers between finger sticks and scans aren’t suppose to match exactly. They should be within 20% of each other though.
It might just be a bad sensor?
Could also be his body chemistry isn’t suited to the Libre. It does read interstitial fluid, and readings can be influenced by inflammation (from application) for any number of days. Though that’s more rare.
@EusticeTheSheep continued with the discovery (for me) of @Sprague, Richard Sprague:
Comparing CGM with Finger Prick.
I thought of pasting in an excerpt but anyone seriously interested should read the post and see what he did and said. It sounds sane and useful to me, though again I’m not expert.
@Sprague replied several hours later, re the 50% variance reported above:
“Wow, that’s pretty extreme. My guess is you got a bad sensor; maybe 20% of mine fail for whatever reason, often because I inserted in a non-fatty part of the arm.
“Sometimes takes a couple days to calibrate correctly. Never, ever medicate without finger test.”
I posted about this on Facebook yesterday. You can read all the replies there, but here I’ll paste in some that seem useful.
First, from the remarkable and generous Ted Eytan MD, who has more than once turned out to be right when everyone else was wrong:
“The freestyle does not measure blood, it measures interstitial fluid – it’s amazing but you have to know its limitations – there’s a delay in reading + it can be affected by vitamin C ingestion.
“It’s not really intended for any sort of closed loop or rapid titration of insulin. For that the Dexcom (much more $$$) is a better choice.
“I’d advise following Richard Bernstein, MD’s YouTube channel – he frequently goes over the topic of blood sugar testing – even a standard meter can be +/- 20 %. (I’m giving this info as a person who’s used this device for almost 18 months – 45,000+ readings – I can tell you what my glucose was at any moment in my life :-))”
Continued –
In response, frequent commenter Susan Eff replied about Bernstein:
“Ted Eytan the best thing about doctor Bernstein is he pioneered the use of personal meters for glucose testing and he pioneered the empowerment of using it to control one’s diabetes with or without meds or with diet alone.
“He was an engineer married to a family physician who was following the advice he’d always gotten as a young person to control his type 1 diabetes but he was never in good control so he applied his engineering mind to the problem went to medical school trained himself in endocrinology after getting his family medicine training and became an MD.
“What could be better for sweating the details than an engineer turned MD who actually cares about unbiased measurable results and patient empowerment?” (I answered: what could be better is if he also generously shares what he learned, aka a YouTube channel!)
Continued
Ted continued, “Everything you need + definitely buy his book – he has an amazing back story – diabetes type 1 before there was such a thing as glucose testing and medical care was doctors telling patients “you’ll go blind and lose your kidneys, so eat what you want”
https://www.youtube.com/c/DrRichardKBernstein/
[Me: yikes]
continued
Ted again, to Susan:
“one of the most meaningful parts of wearing a CGM (which is easy to spot) are the number of people with diabetes who approached me to compare notes & the stories of how they are treated by their doctors are heartbreaking.
“It feels a bit like being a spy but on the other hand to experience some of what people with diabetes do is a gift every doctor / health professional should experience.”