I have a new diagnosis. This post starts with a little history for context.
Ten years ago, three years into evangelizing patient engagement based on my kidney cancer story, I posted Time to practice what I preach: I have skin cancer again. Noting the pattern that highly engaged patients everywhere follow, I blogged that it was time to …
Connect with a patient community, if I can find one.
Learn what I can about the disease: what is this disease, anyway? What goes wrong in it?
Assess my treatment options. …
Of course the stakes with kidney cancer are far higher than a simple skin cancer, but the principles are the same: the person who has the problem (the patient) has every reason and every right to understand what’s going on, understand their options, choose their own priorities, understand their status, and generally be involved (engaged) in the whole process, not be a passive sock monkey.
It’s important to understand that this isn’t “just” a cultural movement: it’s a legit movement sociologically because it can alter outcomes, so if we squelch it, we’re holding back progress. Specifically for me:
- After my kidney cancer, my oncologist said in the BMJ, “I’m not sure you could have tolerated enough medicine if you hadn’t been so prepared.”
- In my skin cancer, survival wasn’t the issue, but I ended up choosing a treatment that was just as good (to me) and cost me 90% less, but which had not been offered until I asked.
In both cases I had to think what I wanted, ask, learn, and keep at it. That’s called being empowered and engaged.
With that as context, now this, 2021:
Glaucoma

In summer 2020, cataract surgery on my left eye went wrong: lens fragments got loose. I needed to have the eyeball vacuumed out (aka vitrectomy), and long story short, that eye will never be right. (Today my glasses prescription is complicated due to the replacement lens not being at the right focal length. I no longer have one pair of glasses that works at all distances.)
This January I developed a new symptom in the same eye (Facebook discussion w images). My local ophthalmologist in Nashua NH diagnosed CME … cystic macular edema. (A cyst in the macula (a part of the retina) was causing swelling (edema). Understandably, a wrinkle in the retina causes ripples in the vision. Not Good. He prescribed drops, including steroids, to reduce the swelling.
After the surgical failure and then this, I decided to transfer to a downtown Boston practice. The retina specialist there added, out of the blue, that I appeared to have glaucoma. Lovely! (Specifically, I’m diagnosed with steroid induced glaucoma: caused by those eye drops. Apparently I’m in the 5% of patients whose eye reacts strongly to steroids.)
At the time I didn’t have much to say publicly so I just started compiling notes and thoughts on a new, unstructured glaucoma page on this site, as I tried to do what engaged patients do: learn about the disease, understand what I can.
If you review that page you’ll see what it’s like to be a troubled stranger in a strange land: out of nowhere I’ve lost 30% of the vision in my left eye (forever), I have weird conditions and terminology to learn, it’s really hard to get questions answered, and I can’t even get the damned eye drops to dispense right. (Eye doctors have no standard, evidence-based way to teach us, for how to dispense drops!) And I cannot get help.
So again the most important thing to me was to find a community of people like me who were savvy. During my kidney cancer, the community on ACOR (now SmartPatients) played a vital role in helping me understand what’s going on, and they were available 24/7, unlike my doctor’s office. Most important, they saw the issues the same way I did, and had years of experience knowing what matters. And I just couldn’t find such a community. (The best I could find is some little groups on /reddit.)
And then, good news, bigtime, times two.
1: The FitEyes patient community
I found a patient-created website, FitEyes.com, with its companion sites discuss.fiteyes.com (an email group) and a new question-answer site they’re developing called Ask.FitEyes.com. The Discuss site is exactly like what I had on ACOR: pretty much a mailing list, with archives so you can search for old topics. Like ACOR, Discuss has savvy senior members and some completely new.
But a mailing list has limitations – it can be really hard to find the good stuff that happened two years ago, etc etc etc. That’s why for years they’ve been working on the Ask.FitEyes.com addition. It’s a work in process, driven entirely by what the patient community needs. I think of it as a highly curated/massaged resource library
You’ll see that FitEyes makes no attempt to be a glitzy upscale “buy the owners a Tesla” website, because it’s not here to please investors, it’s here to be whatever patients need.
FitEyes is fifteen years old and nobody’s heard of it and it doesn’t pop up if you google for glaucoma patient groups. I hope to help it become widely known.
2: Home eye pressure monitoring (“self-tonometry”)
This is a crushingly important development.
Managing glaucoma is all about monitoring your eye pressure, because if pressure gets too high it kills retinal cells. (And they never come back. That’s what happened to me.) And until recently you could only check your pressure in the doctor’s office. That’s disastrous news – your pressure could be dangerously high, but without a machine, you’d have no way of knowing!
This is exactly the situation that used to be faced by people who have diabetes, until they got the ability to do their own finger sticks at home. Before then they could only get checked during a doctor visit, and in between, things would be completely out of control. It also reminds me of my friend Hugo Campos, who has an implanted defibrillator for his cardiac condition, but his doctor held the device’s data, and Hugo didn’t. So in between, he’d be wondering, “What’s going on with my heart right now??? Am I in danger right now??? What was that I just felt??”
Similarly for me, day after day I’d be wondering, “What’s going on in my eye?? Right now??? Is this ouch I’m feeling a problem?? Is the pressure high enough that more nerve cells are dying??” But not even my doctor had the data, because for eye pressure there ain’t no data when you’re not in the office. Knowing eye pressure requires a tonometer – a device that can check the pressure (the “tone”).
Now there’s this: home tonometry – machines you can use at home. And I got one. It’s far from cheap – $2800 – but we are on the pioneering edge of a new world, and things cost more when they’re new. I’m gonna use it and I’m gonna share what I learn.
My new iCare Home handheld tonometer
Here’s a one minute video of what it looks like and how it works. (YouTube selected a freaky frame of the video for this preview – sorry!)
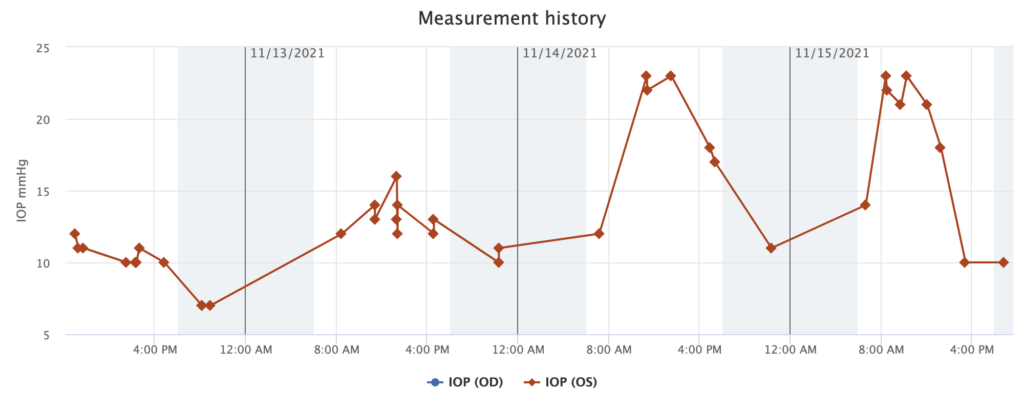
To gather the data, it comes with a little Android tablet that acts as a go-between from the device to the cloud. (I guess if you have a PC it will plug in directly.) Here’s a snapshot of the data I’ve collected so far:
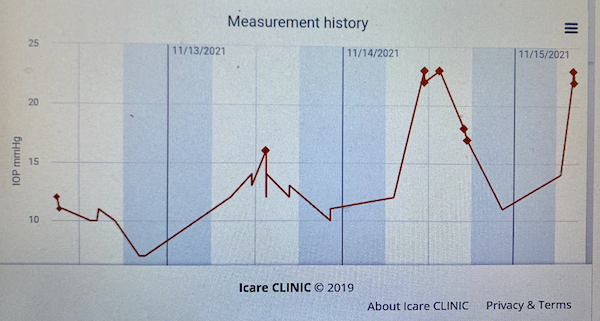
Most of my early readings have been in the range 10-14. (“Normal” pressure is about 12-22.) The highest my docs have recorded has been around 30. What are these spikes yesterday and today of 21, 22, 23? They’re after my beloved strong morning coffee!
The FitEyes community says some people’s eye pressure is super sensitive to caffeine; others aren’t. Looks like I’m one. (Is it related to my similar strong reaction to steroids??)
And here’s the thing: I would never know this, based on the readings I get in the doctor’s office.
iCare is a Finn company. Unlike some medical device companies, they let me have every bit of the data from my readings and do anything I want with it. Woohoo!
It’s called diurnal variation
It turns out your eye pressure can go up and down all the time, all day: so-called “diurnal” variation (i.e. “through the day”). The entire normal range 12-22 is just ten points, but diurnal variation can be that large. (Not usually, but it can.) So how do you tell, from any one pressure reading, whether it’s as high or low that day as it looks??
Some people’s pressure typically starts high and reduces through the day; a few people start low and rise through the day. And as mine illustrates, some people are really sensitive to caffeine or other factors.
So it just seems ridiculous that the norm is just to record the pressure and date, without putting it in context – and to make treatment decisions on the basis of comparisons between two dates, without comparing context and norms.
On top of that, patients on FitEyes discovered through self-measurement that just like blood pressure, there’s a “white coat hypertension” effect for eyes: their own readings with their own devices can be substantially higher in the doctor’s office.
And these shaky-pudding readings, with all their confounding variables, are the foundation of most glaucoma treatment decisions.
(Apologies for all the italics. I just get exasperated when I learn important stuff that wasn’t presented right up front and which is really useful to know.)
This is just the beginning.
Let’s be clear: this is important to me. I have no interest in losing more of my vision. I want my eye health to be managed successfully. And that means knowing what I can about my eye pressure.
Economics has been called “the dismal science,” a phrase that’s echoed in my ears month after month as I sat through visit after visit where another isolated pressure check or reading would be done, and another seemingly random round of prescription eyedrops would be doled out, with no clear sense of exactly what the strategy was. “Let’s try this now, and I’ll see you in a month or two.”

Eye pressure is mainly treated by controlling the many factors the affect the flow of fluid into and out of the eye, and nobody really knows which one you specifically need. So I’ve ended up with prescriptions being tried, paused, restarted, represcribed. (Photo shows my current cabinet of unused, discontinued eye drops, not including the ones I’m still on, and my insurance didn’t cover most. Waste.) We try something, and check pressure weeks later, and if that check doesn’t show progress, we try something else.
Ugh: this is a science?? Seems to me that being a glaucoma specialist is the real dismal science.
The outlook is as good as possible.
Regular readers know that although I can be exasperated, my constant goal is to achieve the best possible outcome, as an informed / engaged patient partnering with medical professionals. As I’ve often said in speeches, I want healthcare to achieve its potential in every case, and we can’t do that if resources are left undiscovered.
I am science-based: I like evidence, experimentation, careful thought. I’ve also blogged for years about the need for e-patients to understand science’s limitations and to not stop at the literature, which can lag years behind the latest best practice. So you can imagine that I want to understand the relative quality of home devices compared to “real” in-office machines.
So this morning I got my pressure checked at the Nashua eye doctor (with two different devices) and compared it with my iCare Home. Results vary widely, which doesn’t surprise me because of the FitEyes articles below: (left eye only)
And you can imagine how fascinated I was to read these two articles on Ask.FitEyes:
- Is Goldmann Applanation Tonometer (GAT) the Gold Standard? (In short, precisely measuring eye pressure is messy at best, and the answer is no)
- Is the iCare HOME tonometer effective for monitoring treatment changes recommended by my glaucoma specialist? Yes – and this is really important, because you don’t have to be a perfect device to be useful for monitoring changes between visits.
Game on.
p.s. By 7 pm the pressure seems to have recovered from the coffee.


Very interesting, thank you.
Yes, I agree with the “let’s try this and come back in 2 months” lunacy.
I believe my right-eye glaucoma came from steroid drops taken after a retinal detachment.
Hi Nicki – as I imagine you know, the community on FitEyes suspects the actual incidence of “steroid sensitive” eyes is much higher than the 5-10% I’ve heard mentioned as a supposed norm.
Some longtime savvy members say it might be as high as 20% or even more. Note, this is NOT a validated published study – the whole problem is that we don’t HAVE good validated scientific studies of the subject.
And that’s part of why we’re on our own to do what we can, while science does its best to catch up someday…
I find your journey to be fascinating and inspiring! Do not let up.
A new treatment which you might benefit from is the MicroPulse MPTLT device. A discussion amongst Drs who have been experimenting with its use was held 11/6/21 and is published at IRIDEX.Com under the Physician Education tab. It is not so much that the treatment is applicable to your case, though it might be, as it is the way the Drs candidly discuss the experimental process. Glaucoma is a window into so much, just as the eyes are the window to the soul! Although the video is almost 2 hrs, it would be very much worth a look.
Dave, very sorry to hear about your latest troubles, but you ARE an inspiration to me as I wrestle with my own. Thanks for this blog. It’s amazing.
Same to you, Brenda. Everything we’ve all worked on for ten years (and more) really does come down to doing our best to have healthcare achieve its potential in every case. You exemplify that as much as anyone!
A FitEyes member emailed this response:
_______________
The “try and see” approach with the glaucoma drops (your collection is pretty impressive..) is something that is really hard to deal with.
I could not use latanoprost. It made me completely sick immediately.
Doctor switched to Alphagan P. He did mention that there may be side effects along the way ~ “in a few months”.
Recently I started having recurrent corneal erosions.
Happens at night, I can’t open my eyes, then sharp pain in the eye and the long process of trying to recover from it.
Considering that I work and have to be *on* for the meetings and brainstorming sessions with full focus on the computer — it is really not easy.
I had to discontinue drops.
I find FitEyes an amazing resource and real support that is so needed.
Thanks for sharing, Dave. You inspire, again. All sorts of vision issues. Mine is double vision at a distance. That distance changing during the day. Now have 4 pair of glasses. Reading music has been a challenge. Changing lots of habits. Hadn’t thought about relevant communities. Thanks for reminder to reach out.
FitEyes isn’t just for glaucoma! They had an amazing thread yesterday on dealing with dry eyes. (Example: DryEyeShop.com)
Funny what happens when you gather a group of people who share a concern, huh???
Dave, this is Brenda Denzler. I’m trying to email you privately to discuss something, but I seem to have lost all of my email addresses for you. Can you get in touch with me via email?
Brenda